Liberty Protection Safeguards – Will you be ready?

Lisa Lloyd – NHS Managing Consultant, Health & Social Care, Practicus
Setting up Integrated Care Systems (ICS), with the appropriate leadership in place, is not the only challenge confronting NHS Leaders. There are also a number of micro transformations taking shape, with April 2022 as a hard deadline for being operational and functioning. One such micro programme is the transformation of Mental Health Services. This includes the Mental Capacity (Amendment) Act 2019 (MCA), which introduces a new framework––the Liberty Protection Safeguards (LPS) designed to replace the existing Deprivation of Liberty Safeguards (DoLS).
The expectation today is that LPS will be implemented across the newly ICSs by that date, as part of an overall MCA strategy. This means NHS organisations such as Hospital Trusts, CCGs and the new Integrated Care Boards (ICBs) need to be putting firm plans and people in place to address how their organisations will meet the need and demand in their area. This is the time when a skilled project planning expert with extensive understanding and experience of Patient Safeguarding and MCA and DoLS legislation in particular, could make a valuable contribution, even on an Interim basis.
WHY A NEW LPS SYSTEM
LPS will apply to England and Wales and aims to streamline and expand the existing DoLS provisions currently in place. Streamline to make it less bureaucratic, while extending eligibility to new groups, namely 16 and 17-year-olds, and those in non-residential care settings.
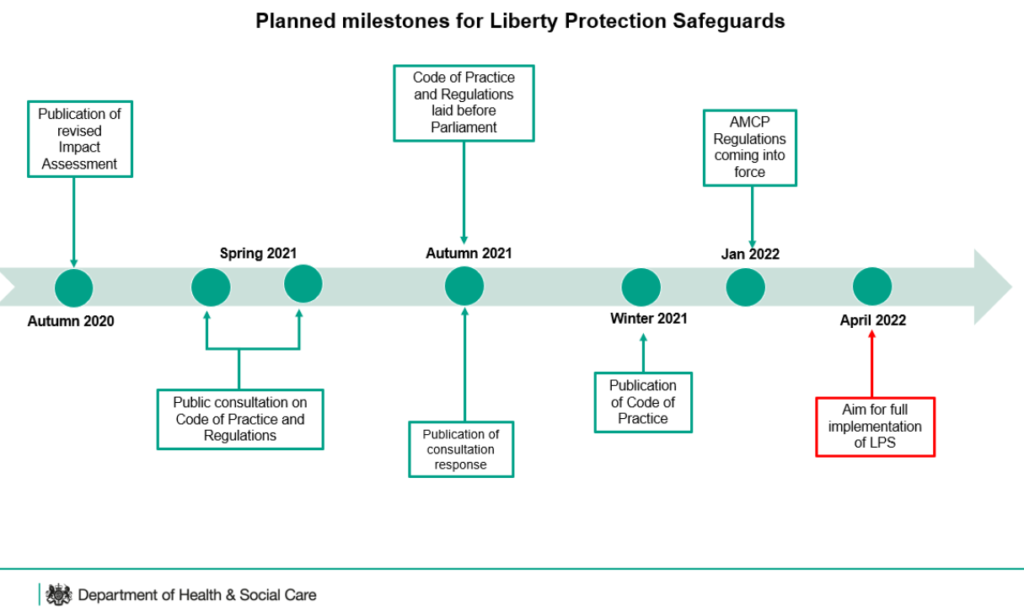
DoLS were due to be replaced by the LPS in October 2020, as part of the Mental Capacity (Amendment) Act which became law in May 2019. Due to the impact of the pandemic, the Government recognised that more time would be needed and delayed implementation until April 2022. However, a lot will need to happen before DoLS are fully replaced by the LPS. (See the DHSC timeline below).
Various regulations need to be written to accompany the Act. These cover topics such as training for Approved Mental Capacity Professionals (AMCPs), transitional arrangements and who will regulate the LPS scheme. At time of writing the health sector is awaiting the publication of a new Code of Practice with a 6-month gap between the final Regulations, being published, and the implementation of LPS.
(And remember, the Code of Practice for the main Mental Capacity Act is also being revised at present).
WHAT ARE DOLS / LPS
Under law, you can deprive someone of their liberty, in certain circumstances, when authorised health and care professionals, in consultation with a person’s family and/or advocates, agree that person lacks capacity to make decisions in their best interests.
DoLS are designed protect people who cannot consent to their care arrangements in a care home or hospital setting. They were bureaucratic to set up and have been subjected to some high-profile court challenges which are the root cause for some of the changes. LPS have the same goals, but with the aim of making them simpler to apply for and administer. It is worth noting that DoLS will run alongside LPS for a year after implementation to ease the transition of existing cases.
The introduction of LPS is a critical area requiring people with the right knowledge to be able to develop the right strategy and operational framework, as well as the detailed implementation plans. If these skills are not readily available in-house, engaging Interim support is a good option to ensure the timescales are met.
UPGRADING FROM DOLS TO LPS
The aim of the LPS scheme is to spread responsibility across hospitals, Clinical Commissioning Groups (CCGs) and social care so as to share the administrative burden, whilst also building the LPS process into the care planning procedure itself. There are proposals to use similar but simplified assessments to the current system but with independent authorisation by an Approved Mental Capacity Practitioner (AMCP) limited to more complex cases, rather than a Best Interest Assessor (BIA), who has previously been involved in all cases.
The LPS is the new way for authorising arrangements giving rise to a deprivation of liberty to enable the care and treatment of people who lack capacity to consent. The LPS will provide safeguards on a wider scale and across a much more diverse range of settings than traditional detention frameworks linked to mental disability. Accordingly, the LPS are designed to be more flexible, and grant detaining authorities considerable discretion in how they perform this safeguarding function.
The main points of the LPS are:
- One scheme will apply in all settings (e.g., care homes, nursing homes, hospitals, supported living, people’s own homes, day services, sheltered housing, extra care, Shared Lives etc).
- Will apply to anyone aged 16+.
- The “Supervisory Body”, which authorises deprivations of liberty is being replaced by the “Responsible Body”. There will be different Responsible Bodies in different settings. For some cases the Responsible Body will be the NHS Trust; in other cases, the role will be filled by the Clinical Commissioning Group (or Local Health Board in Wales); and in other cases, still it will be the local authority.
- LPS will be based on only be 3 assessments:
- “Capacity” assessment
- “Medical” assessment to determine whether the person has a mental disorder
- “Necessary and Proportionate” assessment to determine if the arrangements are necessary to prevent harm to the person.
- More complex cases will be handled by AMCPs.
There will be an expansion of the role of the Independent Mental Capacity Advocate, specially trained experts who can support those not able to make certain decisions for themselves and do not have family or friends who are able to speak for them.
WHO IS IMPACTED BY LPS?
According to the DHSC’s own LPS Impact Assessment, it is envisaged that the LPS will authorise more than 300,000 detentions annually in England and Wales. These affect predominantly older adults with dementia and a variety of people, including younger adults with intellectual disabilities. The largest affected group will be adults living in residential care, or nursing homes, but the LPS will also apply to many adults living in private homes, including ‘supported living’ accommodation.
Applying these Safeguards should not be seen as something separate from providing core health services. It is integral to the measures a hospital must take to protect and promote the rights of people who use its services. Auditing the use of the Safeguards should, therefore, be part of an organisation’s quality improvement programme covering policy, audit, staff training, patient information, relative involvement and reporting on numbers of applications and outcomes. How the Safeguards are managed and implemented should form part of a hospital’s governance programme. These are all indicators that appropriate professionals are required.
WHY HIRING AN INTERIM COULD BE THE SHORT-TERM ANSWER
The need to set up processes to handle the transition from DoLS to LPS by April 2022 is well-established, which suggests people with the right skillset will be in short-supply. At a time when much of the detail surrounding the new regulations have not yet been fully published, there is a definite sense within NHS organisations, that we need to make progress towards the new LPS environment and goals, while still awaiting clarity on some of the details.
At Practicus, we are increasingly helping NHS CCGs and Trusts find the project and programme managers with Patient Safeguarding experience to support readiness planning. Hiring an interim manager does not serve as a replacement for a permanent member of staff. Interim managers are generally engaged for a specific project or initiative, providing on-demand and as-needed support for complex challenges or strategy. They are hired to deliver a specific scope of work to align with project needs. They can of course also be engaged to handle operational workloads, where knowledge or workforce gaps exist.
So, as you contemplate how best to deliver your LPS requirement, if you think you could do with an extra team member to support the development and implementation of safeguarding practice across your organisation, while ensuring effective multiagency liaison and training on safeguarding, then get in touch. We have a deep network of Interim Managers with a wide range of skills, and may just be able to help keep your LPS programme on track.
SOURCES:
The DHSC has LPS materials, and has created a dedicated LPS document collection page.

Lisa Lloyd,
NHS Managing Consultant
Health & Social Care, Practicus
LinkedIn
Our unrivaled client and candidate support have made us the first choice for healthcare appointments. Get in touch if you wish to find out more.
